 In a previous article we discussed how our research uncovered a link between headache and sleep disorders, and how sleep related breathing disorders, left untreated, led to a high incidence of cervical radiculopathy (pinched nerve in the neck) – and then to migraines in those predisposed to them ( See poster on the association between headache, sleep disorders,and cervical radiculopathy). Now we show how Restless Leg Syndrome and Back Pain are related.
In a previous article we discussed how our research uncovered a link between headache and sleep disorders, and how sleep related breathing disorders, left untreated, led to a high incidence of cervical radiculopathy (pinched nerve in the neck) – and then to migraines in those predisposed to them ( See poster on the association between headache, sleep disorders,and cervical radiculopathy). Now we show how Restless Leg Syndrome and Back Pain are related.
The analysis of our electronic medical records data, merged with our digitized sleep center database, showed that sleep disorders can lead to cervical radiculopathy. However, when we began looking for an association between lumbar radiculopathy (pinched nerve in the back), we didn’t find sleep disorders as a major underlying cause. Yet we did find a striking relationship between Restless Legs type movements (a sleep disorder) and back problems. Finding this connection between Restless Leg Syndrome and back pain is a key discovery toward finding relief for these patients.
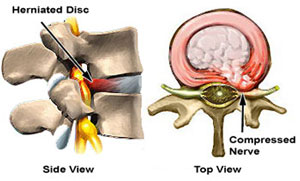
Webster’s Online defines radiculopathy as: irritation of or injury to a nerve root (as from being compressed) that typically causes pain, numbness, or weakness in the part of the body which is supplied with nerves from that root.
Patients with Restless Leg Syndrome and Back Pain had a high incidence of lumbar radiculopathy.
Put simply, we found that patients with lumbar radiculopathy (LR) tended to be awake more throughout their sleep study than those without LR, and many had abnormal leg movements that corresponded with the side of their radiculopathy.
The implications of this finding could be substantial to those suffering with RLS or PLMD who are commonly treated with powerful dopaminergic agents (like ropinerole or pramipexole), drugs used to treat symptoms of Parkinson’s disease and cerebral palsy. These drugs may be heavily overused in patients with Restless Leg Syndrome secondary to other causes, like problems with the nerves going from the back into the legs.
Evaluating a possible lumbar radiculopathy
Low back pain is the second most common symptom-related reason for seeing a physician in the United States, affecting up to 85% of adults at some point during their lifetime. There are many causes of low back pain and most resolve with rest and time. In any case of acute lower back pain we suspect a radiculopathy, and this diagnosis is especially likely if they also have one-sided numbness and tingling in a leg, foot, or toes.
With this type of patient the questions we try to answer are:
- Exactly where is a nerve being affected?
- How severe is it?
- What likely led to this?
- What is the best option to fix it?
MRI, or magnetic resonance imaging, is ideally suited for determining exactly where the nerve root(s) are being irritated, since MRI shows the soft tissues of the body better than any other test. But X-Ray and CT show bones the best. For instance, a herniated disc between the 4th and 5th lumbar vertebral bodies (bones) would show up beautifully on MRI films. But we need to know the structure of the surrounding bony structures, and we need to have an objective measurement of how badly a nerve (exposed to various stresses throughout changing positions of the body through the day) is injured. That’s where an EMG comes in. An EMG will tell us whether the “wires” in the nerves are injured, and how badly.
So you can see that the MRI (coupled with X-Ray or CT) is very specific in pointing out where and what the potential problem is, but neither test shows us how severely the nerves are damaged. Only an EMG, coupled with the clinical history and exam, can answer this question.
Likewise, an MRI is not good for ruling out other causes of nerve involvement, and whether a symptom is part of a more generalized sensitivity of the nerves to damage, as in peripheral neuropathy caused by a host of diseases, including Diabetes Mellitus.
At RNI we learned that appropriate physical therapy can help patients avoid many types of surgery. And physical therapy can many times prevent post-surgical re-injury. We realized that when surgery is done, even appropriately, it is only the beginning.
The solution to low back pain is never an easy process, but with an exact diagnosis and all the information in front of us we realized that only then could we begin to make an individualized treatment plan based upon all the necessary information. Physical therapy is often a good place to start, once you know what you are treating.
Physical therapy is a broad discipline, however, and all PT’s are not alike. We realized that PT must go hand in hand with treating providers, and communicate, almost on a daily basis, with those providers. That is why we at the RNI had a P.T. practice with three highly-trained DPT’s on staff. These providers taught us a much as we taught them, and our cooperation allowed us to deliver, as a team, care at the highest level for neurologically impaired patients with all types of disorders.
We see many folks starting to get better after just a few sessions of appropriately directed physical therapy, when months or years of chiropractic only alleviated their symptoms temporarily. Similarly, we have found other PT programs don’t always arm patients with the knowledge they need to continue keeping themselves out of trouble for the rest of their lives. In the Kansas City region, our tradition is carried on by Drs. Shane and Brandi Jackson, at Optimum Physical Therapy, in the Northland.
Most patients with lumbar radiculopathy could benefit by losing excess weight. This is a societal problem affecting more than just those with low back pain. Ironically, if back problems are causing sleep problems, as our research shows, overweight patients are facing an uphill battle, since increased body mass indicates a higher risk of both back pain and sleep disorders.
More and more scientific research is finding that poor sleep quality hampers the body’s ability to regulate insulin, and this inevitably leads to obesity and Type 2 Diabetes Mellitus. And many other factors are now realized to contribute to obesity and disorders of appetite control, and endocrine disorders like Hashimoto’s Thyroiditis. The role of the gut microbiome in these and other pro-inflammatory disorders is increasingly being realized. Thus back pain is never a simple problem, but requires a multidisciplinary approach for improvement of quality of life. Surgery by itself is rarely the answer to such a complex problem, and often makes it worse.
 Besides having board certifications in both Neuroimaging and Electrodiagnostic Medicine, Dr. Vernon Rowe is board certified in Sleep Medicine, and Neurology. These qualifications are unique among neurologists in the US, why his team was the first to discover the relationship between lumbar radiculopathy and RLS/PLMD.
Besides having board certifications in both Neuroimaging and Electrodiagnostic Medicine, Dr. Vernon Rowe is board certified in Sleep Medicine, and Neurology. These qualifications are unique among neurologists in the US, why his team was the first to discover the relationship between lumbar radiculopathy and RLS/PLMD.
This series originates from a Grand Rounds presentation to Neurology and Neurosurgery residents and staff at the University of Kansas Medical Center.