 At RNI we help patients avoid surgery for pinched nerve neck pain by aggressive Physical Therapy to correct a posture problem that continues to put strain on the neck and cervical nerve roots.
At RNI we help patients avoid surgery for pinched nerve neck pain by aggressive Physical Therapy to correct a posture problem that continues to put strain on the neck and cervical nerve roots.
Surgery is traumatic, no matter how well it is performed, and pinched nerves causing neck pain respond poorly to trauma. For the purposes of this discussion, conservative therapy includes medications and, crucially, physical therapy by P.T.’s who are expert in neuro-physiology.
Surgery is the last resort for a pinched nerve
There are only three good reasons to perform surgery to relieve neurological problems in the neck, and you’ll notice that two of them are only for cases where conservative therapy has already failed:
- Intractable pain that doesn’t respond to conservative therapy including epidural pain blocking.
- Progressive weakness despite conservative therapy.
- “Long tract symptoms,” where spinal cord compression in the neck causes symptoms in lower parts of the body, with leg weakness, sensory level, and/or bladder problems.
In any of these cases, the thoroughness of the diagnosis a patient receives at RNI will leave no doubt about the nature of the problem and the need for surgery. For these reasons we suggest to any patient with pinched nerve neck pain or other spine-related pain that they see a neurologist before talking to a surgeon.
Why physical therapy is effective for nerve problems in the neck
21st Century humans experience nerve problems in our necks because of how we use, or mis-use, our bodies. It makes real sense that re-training our bodies to move the old-fashioned way would alleviate those problems. Unlike some statements that merely sound sensible, this turns out to be true for the vast majority of cases we see at RNI.
The modern lifestyle requires us to spend a great deal of our active hours with our hands lifted in front of us, doing tasks. Arms are heavy, and over years this arms-in-front posture rounds our shoulders forward and down, and it also bends our upper spine forward. In this forward-leaning posture, the muscles that are supposed to hold the shoulders up are in the wrong position to do so, relative to the direction of gravity. One muscle in particular picks up the slack.
Part II of this article will address how physical therapy can solve the problems described here. The general strategy is to strengthen the muscles of the shoulders and upper back to reverse the rounding and return the upper spine to an upright posture. But to understand why muscles can solve the problem, it is necessary to see how they cause the problem in the first place.
The levator scapula problem

The muscle that holds up the weight of the shoulders when others can’t is called the levator scapula, seen in red in the diagrams. It is in a good position to pull straight up on the shoulder blade, and so this task falls to it when the shoulders are out of position. However, unlike the large muscles that are meant to do this job, it is not attached to a strong part of the spine. It attaches to the three neck vertebrae immediately below the skull, far up and away from the shoulders.
You wouldn’t hang a tire swing from the top of a sapling. But that is essentially what is happening here. The head is a heavy enough burden for our thin necks to support; hanging the weight of the shoulders from its top is a recipe for injury.
The analogy we talk about at RNI is that of a bow (the weapon). The wooden bow begins as a relatively straight piece of wood. The string pulls only on the ends, and its force curves the wooden bow into its gentle curve. The key difference between a bow and a neck, though, is the neck needs to remain straight to do its work.
But why do we let the levator curve our necks backward? Surely there are muscles that could pull from the other side to straighten it?
Unfortunately there is a natural consequence of a forward-bent posture that contributes further to this backward-bending neck tendency, a sort of “second whammy.”
The double-whammy of skull angle
No matter what our bodies are doing, we want to look straight forward toward the horizon. Our eyes want to see out, and our skulls are well-balanced in that position. Even if our posture changes over time, our desire for a horizontal skull angle doesn’t change. So, if the upper back rounds forward over time, pointing our skulls downward, our necks want to bend backward to compensate.
The neck is made to bend backward, but only in moderation. The springy discs between vertebrae have to compress at the back edge of the vertebra to allow this bend, but if the bend is constant they become permanently compressed at that edge, and can even rupture, slip, herneate, etc.
Also complicating matters are the many interlocking prongs and surfaces that protrude from the back of each vertebral body for muscle attachment, and to protect the spinal cord and nerve roots. When the neck bends backward, these structures are pressed closer together, and other tissues can get caught and compressed between them. They also become over-stressed themselves, and can develop their own conditions like inflammation and arthritis.
Remember, these poor discs and vertebrae were already stressed due to their being asked to support the weight of the shoulders in addition to the head. The “whammys” are starting to add up, here.
Over time, this pinching motion of the structures at the back of the vertebrae, combined with the compression of the discs between vertebrae and carrying the shoulders’ weight, makes for some very cramped quarters at the back of the neck. This crowding will cause problems over time on its own, but if the disc begins to bulge or herneate, the crowding becomes acute very quickly with pain and other symptoms.
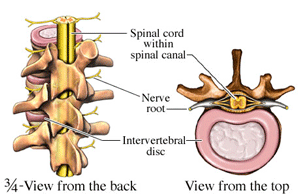
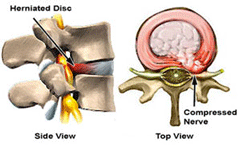 The first tissue to show symptoms is often the nerve root, where a nerve emerges from the spinal cord through narrow gaps in the spine called the foremena. Because a nerve root in the neck is just the end of a wire that serves entire areas of the upper body, sypmtoms can appear in various places. In addition to sensations the patient is aware of, neurologists will check for muscle strength and the presence (of absence) of reflexes to assess nerve impairment.
The first tissue to show symptoms is often the nerve root, where a nerve emerges from the spinal cord through narrow gaps in the spine called the foremena. Because a nerve root in the neck is just the end of a wire that serves entire areas of the upper body, sypmtoms can appear in various places. In addition to sensations the patient is aware of, neurologists will check for muscle strength and the presence (of absence) of reflexes to assess nerve impairment.
Why nerve roots are so affected by these postural problems
In our genetic blueprint, nerve roots were given as much room as they needed to pass out of the spine, and no more. Any extra space is needed to add strength to the vertebrae, which pull double duty as the weight-bearing walls of the body and the protectors of the spinal cord.
Of course, the blueprint was drawn up long before 21st-century humans started bending their necks backward all the time, while at the same time asking their necks to support their shoulders. As the gaps between vertebrae shrink due to flexing and disc compression, the nerves don’t have the room they were promised.
Nerves are extremely sensitive to compression. Their fibers are delicate and have very little protection, and yet each microscopic fiber has its own job to do, connecting one tiny part of the body to the brain. The fibers on the outside of the bundle are the first to suffer any impingement. The resulting symptoms are either pain at the root, noticeably diminished function of the affected nerve fibers, or both.
